By creating a microcosm of the brain on the lab bench, researchers look to gain new insight into diseases such as cancer, stroke, and Alzheimer’s disease.
Project Brainslice gives brain researchers the best of both worlds
By creating a microcosm of the brain on the lab bench, researchers look to gain new insight into diseases such as cancer, stroke, and Alzheimer’s disease.
A brain tumor may not sound like a difficult thing to grow. After all, decades of research and countless careers have been spent trying to stop brain tumors from growing. But with many brain tumors, a funny thing happens once you remove that tumor from the brain itself.
Shawn D. Hingtgen, PhD
“This disease—which is so aggressive and almost unstoppable in a person—fails to grow most of the time as soon as you extract that tissue and try to keep it alive outside the body,” says Shawn Hingtgen, a cancer researcher at the University of North Carolina’s Eshelman School of Pharmacy.
That failure rate can stymie a lot of potential research on brain tumors, from understanding how the tumor cells interact with the rest of the brain to understanding how potential anti-cancer drugs might fare against the disease. But Hingtgen and his colleagues, including fellow UNC cancer researchers Andrew Satterlee and Albert Baldwin, have now developed a new method for growing brain tumors outside of the body with remarkable success.
The secret is to grow them on a slice of rat brain.
A slice of rat brain is exactly what it sounds like: a living sliver of a rat’s brain, complete with neurons and glial cells still arranged in a cross-section of the brain’s architecture and kept alive in a dish. These segments of a rodent’s central nervous system work remarkably well as a medium for growing tumors. And with this technology, the team is working to develop a new form of functional precision medicine, where a patient’s actual tumor could be kept alive in a dish and then tested against an array of cancer-fighting drugs to see which might work best.
That’s just one of the research initiatives now underway via Project Brainslice, a joint effort between the North Carolina Clinical and Translational Sciences (NC TraCS) Institute and the clinical and translational science institutes at Duke University and the University of Florida under a UO1 grant through the NIH’s National Center for Advancing Translational Sciences (NCATS). By creating a microcosm of the brain’s ecosystem on the lab bench, brain slice technology maintains much of the complexity that makes studies in animal or human subjects so insightful, while benefiting from the inherent ease and efficiency of research done in a dish.
For researchers, this creates a “best of both worlds” situation—one that is now being applied across the three universities to study diseases ranging from cancer to stroke to Alzheimer's disease.
Biologists have long had to balance the convenience of laboratory work with the value of working with live subjects. Suppose, for example, a researcher wanted to test how a potential new drug impacts brain cells. By studying that drug in a clump of cells spread on a dish, the researcher can target specific cells and watch them respond in real time, gaining precise data on how that substance affects basic cell biology.
Albert Baldwin, PhD
But in real life, cells don’t live in a plastic dish. They live in the body, alongside all the other cells in the body, corresponding with each other through a byzantine system of hormones, signaling pathways and nutrients. These interactions can change how a cell behaves, meaning what happens in a dish may not always translate to what happens in the body.
Cancer cells and tumors, even if you can grow them outside the body, may not act the same in a dish as they do in the body, either. On plastic, those cells are going to receive completely different signals than they would if they were surrounded by other cells, says Albert Baldwin, a researcher at the UNC Lineberger Comprehensive Cancer Center.
“Once you grow a tumor cell on plastic and do sequencing,” he says, “it doesn’t even look like the original tumor.”
One way of overcoming this problem is to study cells in a living subject, such as by transplanting tumors into mice. But this method also has its drawbacks. Those cells are stuck inside a living thing, so researchers can only get snapshots of what’s happening inside the body by taking samples at different intervals or watching for phenotypic changes.
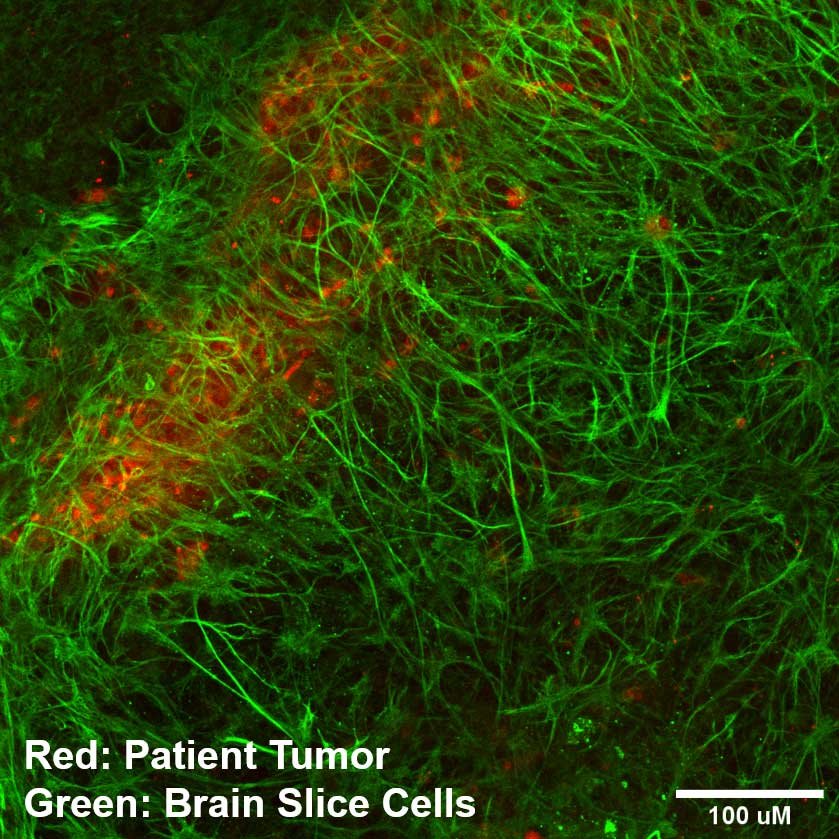
Brain slices could help bridge this gap. By slicing off a thin layer of brain and keeping it alive in a dish, researchers hold onto a lot of the complex structure of the brain, with the brain’s cells arranged much as they were inside the body. This enables researchers to study how these various types of cells interact with each other, which can be much more insightful than studying an artificial monoculture of cells spread on a dish.
In addition, when it comes to cancer, brain slices could enable researchers to see not just how tumor cells respond to certain situations, but also how the surrounding, normal brain tissue responds. And by growing tumors on the brain slice, researchers can study how those normal cells interact with the tumor cells under different conditions.
Andrew Satterlee, PhD
Andrew Satterlee, who has worked with Hingtgen since 2016 and is one of the NC TraCS Institute’s K12 scholars, has seen how useful brain slices can be firsthand. One of his early projects involved looking into why some tumor cells quickly moved around in a dish, in the hopes of understanding how to prevent tumors from migrating around in the body. But inside a body, those cells don’t migrate at all, Satterlee says, but rather grow in a dense ball.
“It made me think: Why would we design a therapy to stop a totally artificial behavior in these cells?” he says.
So, he decided to place those tumor cells on a brain slice instead. And, lo and behold, on the brain slice, those cells grew in a dense ball. “They look and act like they do in the live animal,” Satterlee says.
Don Lo, a researcher formerly at Duke, had been using brain slices for years to study diseases like Parkinson’s and stroke. About a decade ago, he and Baldwin teamed up to use brain slices as a medium for growing tumors, and later, Hingtgen and Satterlee started using brain slices in their research. Now, slice technology underlies a lot of brain cancer research at UNC. This includes the functional precision medicine platform that Satterlee, Hingtgen, Baldwin and others are developing.
The team wants to create a system where a patient’s actual tumor can be excised, kept alive on a brain slice and tested against various cancer treatments. With each drug, a technician would collect data on how that drug affected the tumor cells and the surrounding brain tissue. This data would then be entered in an algorithm to give each drug an overall efficacy score against that patient's specific tumor.
This process still needs to undergo plenty more testing before it could ever be used to help guide treatment decisions. But theoretically, this information could help doctors and patients make a more informed plan of action for treatment with better information on how the actual tumor inside their body might respond to various drugs, rather than guesses based on a handful of the tumor’s genetic markers.
SLiCE Core Facility team
L to R: Rajaneekar Dasari, Breanna Mann, Andrew Satterlee, Xiaopei Zhang and Adebimpe Adefolaju in the brain slice lab.
Recently, the brain slice team at UNC opened a core facility to enable researchers at the university to test their drug candidates on patient tumor tissue. But the potential power of the brain slice technology also goes beyond what’s happening at UNC, and beyond cancer. Other PIs under Project Brainslice at Duke and Florida, for example, have used brain slice technology to study stroke and neurodegenerative diseases like Alzheimer’s, in addition to brain tumors.
There are still aspects of in vivo research that a brain slice can’t replicate—after all, the human body is not a single slab of rat brain. Bodies contain a suite of anatomical systems that interact with each other, like the lymphatic, respiratory and circulatory systems, which aren’t represented in the brain slice. But eventually, slice technology could expand research opportunities in other parts of the body, too. For example, Hingtgen’s lab has also been developing a similar slice technology for mesentery, a type of tissue near the intestines, which could help researchers studying ovarian cancer.
Hingtgen says having researchers at the three universities organized under the same umbrella is useful, especially as it facilitates sharing resources and knowledge. “I think we’re just generally collaborative,” he said.
But this project, he adds, is “designed to help other people”—whether they’re already working with brain slice technology or not.
“If this can help anybody advance their own drug, advance their own trial, advance whatever,” he says, “We would love to partner.”
Photo: patient tumor binding to the brain slice cells — courtesy of Andrew Satterlee
NC TraCS is the integrated hub of the NIH Clinical and Translational Science Awards (CTSA) Program at the University of North Carolina at Chapel Hill that combines the research strengths, resources, and opportunities of the UNC-Chapel Hill campus with partner institutions North Carolina State University in Raleigh and North Carolina Agricultural and Technical State University in Greensboro.


