Esha Agarwal is outsmarting Parkinson’s disease
The UNC undergraduate student is tapping into Carolina's research community to develop an app that could help diagnose the condition.
Esha Agarwal
Esha Agarwal did not ever imagine herself becoming an app developer. "My mom really tried to get me into computer programming," says Agarwal, an undergraduate junior at the University of North Carolina. "I absolutely hated it."
But a few years ago, Agarwal's grandfather was diagnosed with Parkinson's disease (PD). After that, she began to see firsthand how the condition could affect people's lives. And when the COVID-19 pandemic struck in 2020, she saw how hard it suddenly became for her grandfather to go into the doctor's office for regular visits and check-ups.
That's when she had the idea for an app that could help patients diagnose and track their Parkinson's symptoms. Bolstered by the interminable boredom of being stuck at home during the early pandemic months, Agarwal scoured the scientific literature on Parkinson's disease—and taught herself how to code through YouTube videos.
Through this self-guided study, Agarwal was able to develop a preliminary version of her app, which she called "outSMARTPD." Now, as a student at UNC, she's using the resources and expertise of Carolina's research community to take her app to the next level, bringing it one step closer toward helping patients navigate life with Parkinson's.
The whole point of the app is to empower patients to remember that they're still in charge, able to manage their symptoms and live fulfilling lives.
"When you have Parkinson's disease, it's like you're losing your brain, you don't have control over your own body, over your emotions," Agarwal says. "The whole point of the app is to empower patients to remember that they're still in charge, able to manage their symptoms and live fulfilling lives."
For many patients, arriving at a Parkinson's diagnosis is the end of a long and complicated process. The disease—the result of deteriorating function of the brain cells—manifests through a combination of symptoms such as tremors, muscle stiffness, balance problems, and slowness of movement. But the disease doesn't always show up with the same combination of symptoms in each patient. Not to mention, some of the symptoms, such as slowness of movement or balance issues, can also be the result of other conditions or part of the aging process.
"When you're older, it's hard to tell if you're necessarily having symptoms of an illness, or if it's just the aging process, or do you have arthritis, or even a different disease like Alzheimer's," Agarwal says.
In addition, there's not yet any lab test to definitively spot when someone has Parkinson's disease or not. Instead, a neurologist usually sees a person in the clinic, takes a thorough history, and performs a detailed neurological exam to arrive at a diagnosis.
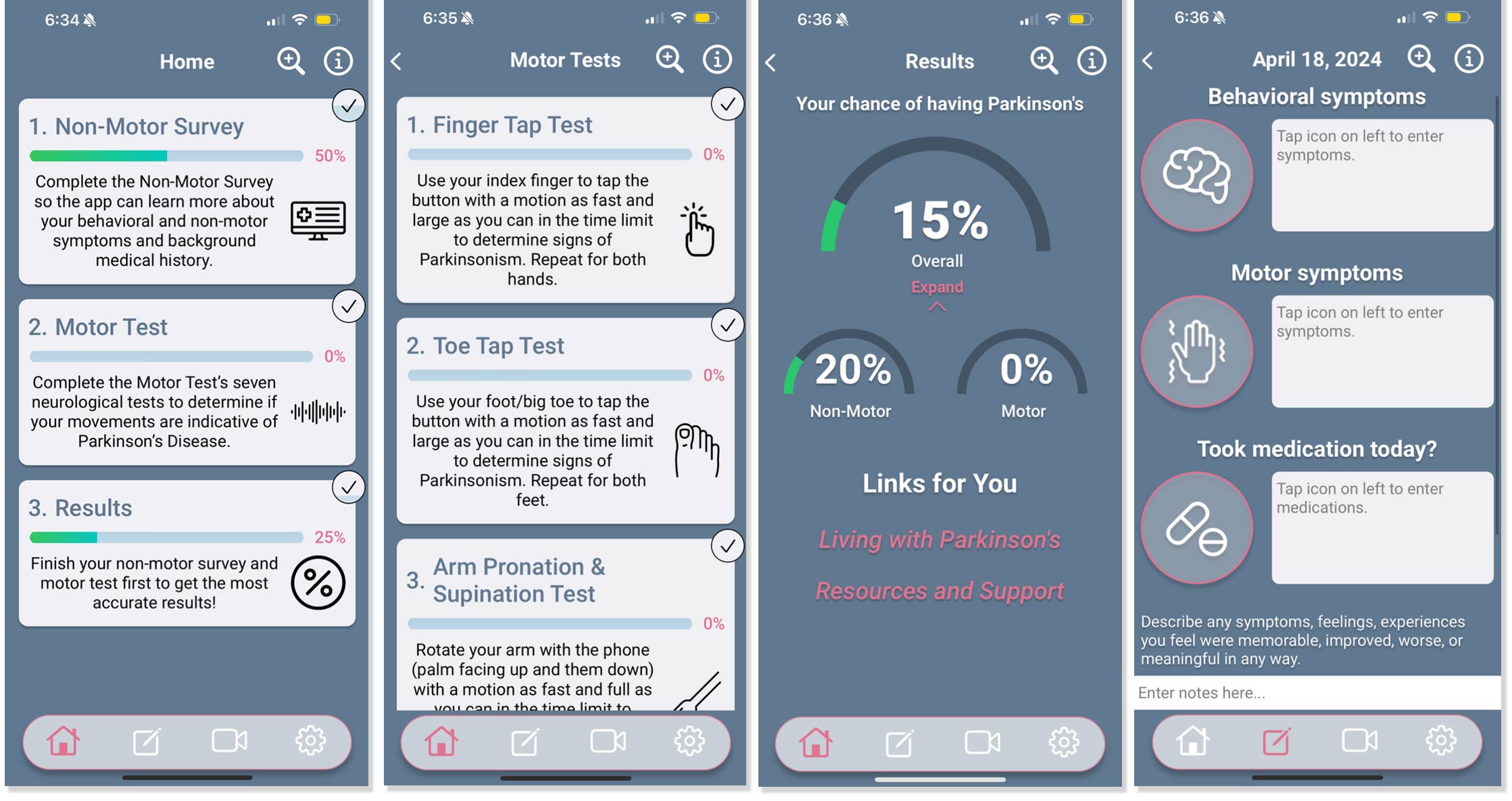
Agarwal has now incorporated some elements of that clinical evaluation into outSMARTPD. That includes physical tests that examine a person's motor function, like one where people tap their finger on the screen as fast as possible, as well as tests that use some of the smartphone's internal tools to check for Parkinson's-like symptoms. For example, one test has people hold the phone in their hand to measure the frequency of any tremor they might have to check if that tremor has a Parkinsonian frequency. The app also includes surveys on a user's mental health and medical history.
From there, outSMARTPD computes a Parkinson's risk score using an algorithm Agarwal wrote, giving patients a sense of how likely it is that they have the disease. In addition, the app offers people links to resources such as Parkinson's research and advocacy groups—and comes with a symptom tracking feature, where patients can note down a particular symptom they're experiencing, keep a log of when they took various medications, or record themselves on video to play back for their doctor later.
Agarwal says the app was initially cobbled together through a simple coding language. But people were clearly impressed, nonetheless. In 2020, she submitted outSMARTPD to the Congressional App Challenge, a competition for youth-created apps hosted by the US House of Representatives. Agarwal, representing her home district in Cary, North Carolina, won first prize. As she moved on to UNC, both she and the app received additional recognition—Agarwal as one of the university's Morehead Cain scholars, and outSMARTPD as a grantee of Innovate Carolina's 1789 Student Venture Fund, a startup development incubator for UNC students.
With this support, Agarwal could fine-tune some of the coding behind the app to help make it a lot smoother and more user-friendly, including through hiring a developer. Last year, she also connected with Andy Kant, the director of FastTraCS, the medical technology incubator at the North Carolina Translational and Clinical Sciences (NC TraCS) Institute. Kant, she says, has become a deeply valued mentor, and encouraged her to connect with Nina Browner, a neurologist at the UNC School of Medicine and Director of the UNC Parkinson Foundation Center of Excellence.
Browner is now serving as the faculty advisor on a pilot study for outSMARTPD, with Agarwal as primary investigator—a key step toward bringing the app to patients. The study has been ongoing, focused on validating and testing the algorithm that determines a patient's Parkinson's risk score. Informally, Agarwal has also been gathering patients' thoughts on using the app. "What's most exciting is seeing how patients respond and react, the impact that app has made for them," she says.
Agarwal sees a variety of potential use cases for outSMARTPD if the app were ever approved. For one, hospitals and doctors could have their patients download and use the app to evaluate and monitor their symptoms, potentially even as part of the intake process before an appointment begins. She also envisions pharmaceutical companies potentially using the app to test the efficacy of Parkinson's drugs in development.
Agarwal's grandfather, who initially inspired the app, passed away this past summer. She says that she's connected with patients by talking about how she developed outSMARTPD to help him—and with luck, that legacy could one day help patients all over the world understand and monitor the symptoms of Parkinson's disease.
But Agarwal also has plans to protect people's health well beyond the scope of app development. Currently, she's majoring in environmental health with a minor in chemistry, as well as completing her pre-med courses. Eventually, she plans to apply to medical school.
"I just love being able to help people," Agarwal says. "The human connection—it's so exciting. It's something new every day."
For more information on outSMARTPD, visit outsmartpd.com.
NC TraCS is the integrated hub of the NIH Clinical and Translational Science Awards (CTSA) Program at the University of North Carolina at Chapel Hill that combines the research strengths, resources, and opportunities of the UNC-Chapel Hill campus with partner institutions North Carolina State University in Raleigh and North Carolina Agricultural and Technical State University in Greensboro.

