The pandemic's impact on primary care Practice-Based Research Networks
Drs. Katrina Donahue, Jacquie Halladay, Michelle Hernandez, and colleagues published in Health Affairs using the analogy of a watershed to explain the primary care system and how the pandemic has adversely affected its Practice-Based Research Networks (PBRNs), a vital infrastructure that provides the capacity to assess and improve health outcomes where most people receive care. Donahue, Halladay, and Hernandez worked on this project as a part of the NC TraCS-supported North Carolina Network Consortium (NCNC). NC TraCS support is key to NCNC's fiscal support for project management, support for practice coaching, and other key administrative functions.
UNC's Katrina Donahue, MD, MPH (Family Medicine), Jacquie Halladay, MD, MPH (Family Medicine), and Michelle Hernandez, MD (Children's Research Institute), along with researchers from across the country recently posted a salient article on Health Affairs "Forefront" titled "The Watershed Of Practice-Based Research: Lessons And Opportunities From The COVID Pandemic."
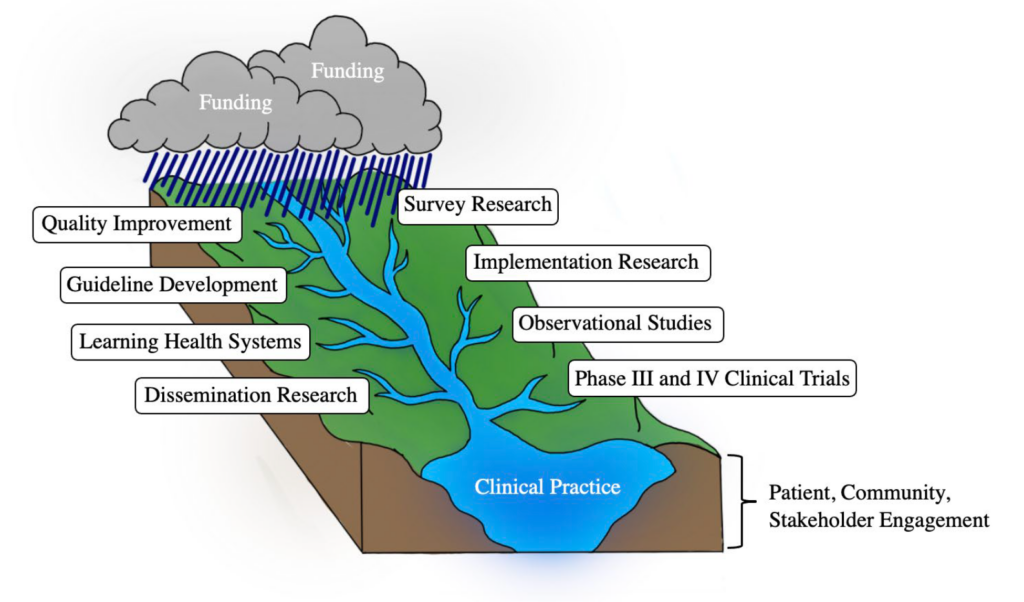
Using the analogy of a watershed to explain the primary care system and how the pandemic has affected it, the post establishes how primary care's Practice-Based Research Networks (PBRNs) are the vital "infrastructure best suited to measuring and improving the health of the national primary care watershed." The primary care system is "where and how most people get most of their health care." Primary care was already suffering large rates of burnout pre-pandemic, with rates continuing as more variants develop. Similarly, PBRNs were already struggling for resources and funding before the pandemic which further depleted much of the limited flow of resources maintaining research infrastructure and capacity.
Donahue states, "Primary care practice-based research networks are critical for addressing and improving health by answering the pressing problems in primary care, where most people receive most of their care. The pandemic has ravaged these networks, leaving the ones that survived on shoestring budgets."
PBRNs that have survived have had to adapt to limited resources, leading to a fragmented system of research also hindering pandemic response. Noting the lack of infrastructure supporting research in health care settings Halladay notes, "These networks can rapidly address pressing issues, such as health inequities and COVID-19 vaccine hesitancy but need adequate resources to do so. Without a dedicated NIH institute or Center focused on primary care, efforts need to be put in place to rethink how to support this critical work."
Read the article at the Health Affairs website.
Originally published at news.unchealthcare.org.