CTSA Program Mentoring Paves Way for Brain Cancer Therapy

Cell biologist Shawn Hingtgen, Ph.D., is convinced that stem cells can effectively treat brain cancer. Using the support he received through the mentored career development program offered by NCATS' Clinical and Translational Science Awards (CTSA) Program, he has collaborated with neurosurgeons, oncologists, stem cell experts, drug development specialists and others to create a potential therapy for glioblastoma multiforme, a deadly type of brain cancer.
Hingtgen, an assistant professor in the Eshelman School of Pharmacy at the University of North Carolina (UNC) at Chapel Hill, previously was an NCATS KL2 Mentored Clinical Research Scholar at the North Carolina Translational and Clinical Sciences (NC TraCS) Institute. Among other things, this award supports mentored career development for investigators who have recently completed professional training and are early in their research careers.
"The multidisciplinary nature of [the] NC TraCS KL2 program enables junior faculty to work with experts in many different fields to solve problems and provide guidance in the process of translating basic science knowledge to clinical medicine," said Kim Boggess, M.D., UNC professor of obstetrics and gynecology and co-director of the NC TraCS KL2 program.
Glioblastoma is an insidious disease that infiltrates the brain, killing approximately 14,000 people annually in the United States. The cancer sends out tendrils into brain tissue that make it nearly impossible to completely eradicate with drugs or surgery. The current therapy for glioblastoma is surgery, radiation and chemotherapy, with most patients only surviving one to two years after diagnosis.
Stem cells are a promising new approach to deal with shortcomings of current therapies. Hingtgen and his team are taking advantage of a technique known as "direct reprogramming." During this process, fibroblasts, skin cells responsible for making collagen and connective tissue, are converted into induced neural stem cells, which have an innate ability to target cancer cells in the brain.
"When neural stem cells are put into the brain, they track down the cancer tentacles and roots that spread through the brain," Hingtgen said.
But that's not enough to kill the cancer cells, so Hingtgen's group has engineered stem cells to carry and deliver drugs to the cancer cells. The researchers are studying two approaches. In one approach, stem cells are modified to carry an enzyme trigger that can activate a drug inside the cells, killing nearby tumor cells. In the second approach, neural stem cells are engineered to carry and continuously pump out tumor-killing proteins that can bind to tumor cell surfaces, killing those cells.
"We're developing a personalized tumor-homing drug carrier with anti-cancer agents that will seek out residual cancer that chemotherapy and surgery miss," he said.
Hingtgen collaborated with a surgeon and an oncologist to create a way to deliver the cells to a tumor site. Instead of being injected, the stem cells are placed on a customized, implantable patch or bandage, which is placed at the surgical site. The stem cells then migrate to the cancer.
While much of the research to date has been done with mouse cells, more recent research has focused on using human skin cells.
Mentoring Improves Research Translation
Hingtgen began his stem cell therapy research as a postdoctoral fellow at Massachusetts General Hospital in Boston. Shortly after arriving at UNC-Chapel Hill in 2012, he was accepted into the KL2 scholar program.
As a KL2 scholar, Hingtgen attended seminars on a range of topics, from how to manage a lab and write grants to understanding the drug development process and therapeutic product development. A mentoring team, including Matthew Ewend, M.D., chair of neurosurgery at UNC Hospitals, helped with all aspects of translation and the product development process for Hingtgen's work. The group frequently met to discuss how to translate the stem cell technology into something useful for patients.
"NC TraCS advisors connected me with surgeons, engineers and others to discuss what a clinical product should look like. We discussed how to personalize the therapy and found a way to get the stem cells into the brain cavity. After several months, we arrived at the first design of our clinical product," Hingtgen said.
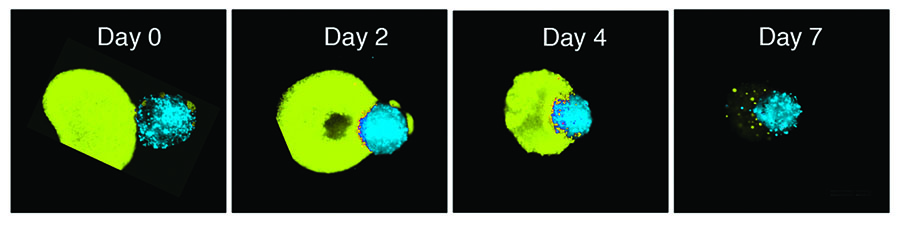
Scientists determined the anti-tumor effects of neural stem cells in 3D culture models. Stem cell aggregates, or spheroids (blue), were placed next to brain cancer cell spheroids. Fluorescent images captured over seven days showed that the stem cell therapy decreased the volume of cancer spheroids. Researchers are working to advance the therapy towards first-in-human clinical trials.
In addition to classroom work, Hingtgen's training and mentoring included work with the NC TraCS 4D (Drugs, Devices and Diagnostic Development) program, which enabled him to consult with experts in pharmaceutical product development to explore commercial opportunities and industry partnerships. At the same time, the joint NC TraCS-Research Triangle International Regulatory Service advised on pre-clinical regulatory requirements for the product. With NC TraCS' guidance, Hingtgen wrote a research protocol and received UNC institutional review board approval to collect human cancer tissue for testing with the experimental stem cell therapy.
Hingtgen received a $50,000 TraCS pilot grant to develop a stem cell bandage, enabling him to partner with research leaders and generate preliminary data that led to a 2016 grant from the National Institute of Neurological Disorders and Stroke to further develop the technology.
Perhaps just as important, the KL2 program specialists helped Hingtgen hone his presentation skills.
"Through the KL2 program, I also met with communications experts who helped me develop a five-minute sales pitch — sometimes called an 'elevator speech' — which helped me land a $750,000 award from the UNC Eshelman Innovation Fund and a $300,000 grant from the state of North Carolina to further my team's research," he said.
The 4D program experts also helped him work with UNC's intellectual property office to file two patents for stem cell work and, subsequently, start a company, Falcon Therapeutics, based on the stem cell technology. The company recently licensed the technology from the university.
Hingtgen is continuing to gather data and refine the stem cell technology, and he is using his elevator speech as a springboard for discussions with the U.S. Food and Drug Administration. He credits the KL2 experience with teaching him the value of collaboration, team building and communication, all invaluable skills critical to his growth as a translational scientist.
"I have always wanted to create solutions in the lab to help improve people's lives," he said. "We're making a therapy that has the potential to help thousands of cancer patients, and our goal is to get it to patients as fast as we can."
Originally posted at ncats.nih.gov.