UNC Researcher Receives NIH Grant to Model Rare and Puzzling Type of GI Cancer
When one hears about a tumor of the gut, the first thing that probably comes to mind is colorectal cancer. It is, after all, the third most commonly diagnosed cancer and the third leading cause of cancer death. Yet, by size, the small intestine dwarfs the colon, making up more than 70 percent of the length and 90 percent of the surface area of the digestive tract. Still, cancers of the small intestine are so rare that only limited information is available on their incidence, prognosis, and treatment prospects.
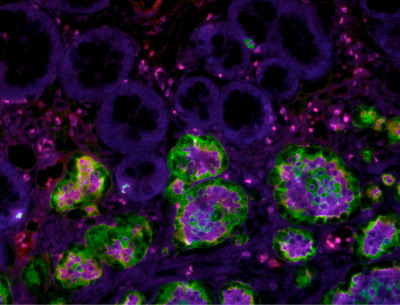
(Credit: Dr. Haydee Lara)
"Nobody really understands why that's the case," said NC TraCS member Scott Magness, an expert of gut biology. "For the number of cells you have in your small intestine, it's shocking that you don't get more cancers like you do in the colon." When cancers do arise in the small intestine, they look completely different, presenting as a rare, slow-growing variety known as neuroendocrine tumors or NETs.
Recently, Magness received a $350,000, two-year grant from the National Institutes of Health to engineer new approaches to study this puzzling type of cancer. Scientists still don't know the types of mutations that generate NETs, or even the cell type in which it originates.
The human gut regenerates its lining every few days, using two types of regenerative stem cells found deep within the accordian-like folds of the intestinal wall. One type of stem cell, the "active" intestinal stem cell, divides quickly and has been implicated in colon cancer. The other type, the "reserve" stem cell, divides much more slowly. That's the one Magness believes is responsible for cancers of the small intestine.
Small bowel NETs are extremely rare, with an annual incidence of only about 0.7 per 100,000. Magness and his team are working with Autumn McRee, a medical oncologist in the UNC Gastrointestinal Oncology Program, to identify patients with NETs who are scheduled to undergo surgical resection.
"The work Dr. Magness and his team are doing is novel and very exciting," said McRee. "Knowing the biologic blueprint of how neuroendocrine tumors develop and spread could provide more effective therapeutic options to delay recurrence after these tumors are resected."
But working with these tiny tumors in the lab presents a big challenge. "The samples are small and the samples are precious, and we want to get as much out of them as we possibly can," said Leigh Ann Samsa, a postdoctoral fellow in the Magness lab.
Luckily, Samsa is an expert at studying biology on small scale, even single-cell levels. During her dissertation, she studied heart development in zebrafish, a remarkable organism that can generate the beating organ from a single cell in less than 24 hours. "You can imagine that the genetic changes that happen during that process are very dynamic," said Samsa. "The same thing is probably true with the evolution of intestinal cancer."
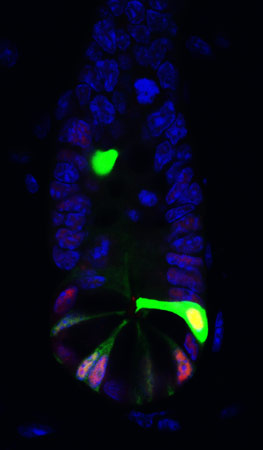
Samsa breaks down each tumor she procures into single cells, and then analyzes each of these single cells to map the constellation of genetic changes that potentially drove the cancer. A number of seminal studies have already uncovered such "driver" mutations in colorectal cancer tumors. Yet no one knows which mutations set the course for small intestinal NETs.
Once she and her colleagues have compiled a number of candidate mutations, they will try to reverse engineer the disease by introducing these mutations into both active stem cells and reserve stem cells. They can then place these mutated stem cells onto a CellRaft Array, a credit-card sized device containing 15,000 tiny wells where the cells can grow into fully developed tissue structures known as mini-guts. Each microwell is stamped with a specific address, so the researchers can track stem cells that are behaving normally and those that seem to be developing cancer characteristics. Those that act like NETs in a dish could then be studied further, or transplanted into mice to confirm their ability to cause cancer.
Ultimately, the researchers want to understand what causes these tumors so they can develop cell culture models for testing new ways to diagnose and treat the rare, but deadly, disease.
"Tumors don't start as tumors, they likely start as a single cell," said Magness. "We want to identify those dysregulated events that happen in a single cell that allow it to grow up and turn bad, to become a tumor. If you knew the pathways that might give rise to NETs, when it isn't a solid growth but only a single or perhaps a handful of cells, then you could identify it early and stop it in its tracks. Before you can even think about those questions, you need to do a lot of discovery-based science. That is what we are undertaking with this research."